Homelessness: A True Public Health Problem
Henry is a typical client of mine. Decades of prison time, sausage-like fingers from too many construction accidents, a toothless smile, and a rap sheet of neuroses and disorders. An archetypal black male, blue collar, criminal deadbeat. Henry started snorting coke and drinking as a kid, mainly as a social way to escape his alcoholic father and depressed mother. He dropped out of high school. His various jobs were like his women, which, in Henry’s world, was an unjust existence: short-lived, cheap, and tossed aside once his drinking became a problem.
Today, I sit with Henry because Henry is homeless. We’re working on filing a claim for disability benefits. Tufts of grey hair sprout from beneath his army cap, and through the ripples of his many jackets and sweatshirts, his chest gently heaves.
We start by going over his medical history, which had primarily been at the hands of prison doctors. Some of his conditions were not only treated while he was in prison, but had developed there. Henry is HIV positive, missing a kidney and a part of his right ear, and has PTSD. In no uncertain terms, Henry attributes his current bill of health to the stunning matrix of “thugs, idiots, and assholes” he encountered at a State Correctional Institution.

Homelessness is a public health issue that remains largely unexamined. It has neither the dangerous appeal of infectious diseases nor the universal attention to childhood illness. The unsavory nature of homeless health issues makes it uncomfortable to discuss: trench foot from being outside in the rain, scabies from mites hidden in unkempt tents, sexually transmitted infections (STIs), untreated mental health issues, and drug & alcohol addiction.
Where and how the homeless get treated for their health issues is a challenge. Lack of affordable public transportation makes it difficult to keep doctors’ appointments. Sporadic jail time introduces changes in prescription medications, other treatments, and clinicians. Lack of insurance is thankfully being ameliorated by some of Pittsburgh’s free clinics and assistance in accessing Medicaid thanks to statewide expansion, yet even the smallest of copays still pose a problem for many people.
With the right care, many serious health risks are manageable. Diabetes II and high blood pressure can be helped with a proper diet, social support, and an active lifestyle. Tending to mental health issues requires the same kind of social support, therapy, and sometimes psychotropic drugs.
A lack of continuous care puts many people who live on the streets on the brink of mental and physical collapse. Untreated, Diabetes II, high blood pressure, and bipolar disorder, among many other health issues, can be fatal.
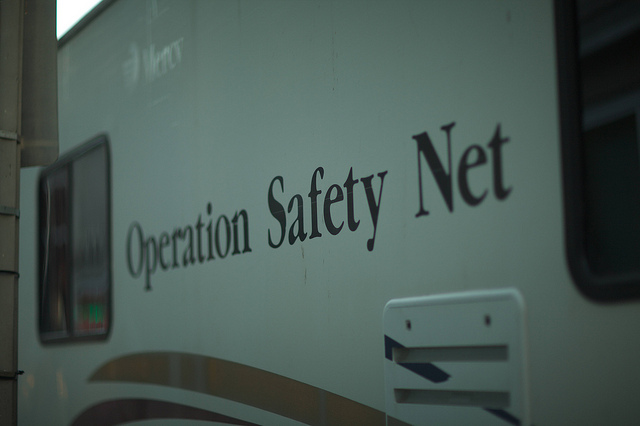
Addressing the disparities in health treatment for the homeless is complicated. There are a lot of social and economic factors that play a part in determining one’s health outcomes, and these risk factors are exacerbated by life on the street. At Operation Safety Net, we serve Allegheny County’s homeless population by leveling the playing field – providing access to medical insurance, a nest of physicians, nurses, social workers, and therapists, and the social support to maintain positive health changes.