Collaboration Improves Patient Care
One in five Americans experience a debilitating mental illness such as depression. Despite having effective treatments for most mental illnesses, many patients are unable to access them. Some of the barriers include a shortage of mental health professionals, the stigma of mental illness, and the lack of affordability. This leads to a majority of patients receiving mental health treatment from their primary care physician (PCP). Unfortunately, many barriers prevent patients from getting better. 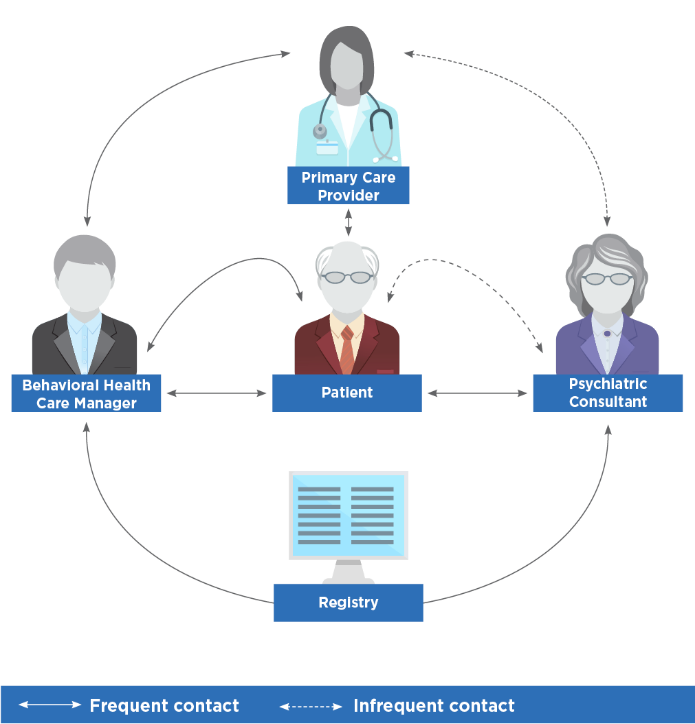
The Collaborative Care Model addresses many of these barriers. It is a patient-centered, innovative approach to integrating behavioral health and primary care services. In addition to the PCP treating a patient’s mental illness, two members are added to the care team: the behavioral health care manager and the psychiatric consultant. The behavioral health care manager is responsible for calling patients to see how the treatment is going, connecting them to resources, and providing counseling. They also use a registry to track patient follow up and outcomes. The psychiatric consultant gives advice to the team about treatment options and helps the PCP develop a plan if a patient is not feeling better.
This year, I’ve been a part of the collaborative care team at the Shadyside Family Health Center as the behavioral health care manager. When a patient is diagnosed with depression, their PCP routes their chart to me to initiate follow-up care. Every day, I conduct mental health check-ins with these patients and collaborate with them on their health goals. My phone calls allow me to identify barriers to treatment, alert PCPs when their patients are not improving, and facilitate communication with our psychiatrist regarding treatment changes. I also meet with our psychiatrist weekly to review treatment plans for patients who need more intensive mental health care.
Our team-based approach to mental health care has prevented many patients with depression from falling through the cracks. In many of my phone calls, patients have expressed to me that they have never had a health center care about them as much as we do. They feel more confident, hopeful, and engaged in their treatment plan knowing that they have a team working with them on their health goals. In fact, one of my patients who recently moved away from Pittsburgh is planning on taking 3 buses to get to our health center, rather than transferring her care to somewhere closer. Her commitment to receiving her primary and mental health care at the Shadyside Family Health Center is a testament to the effectiveness of our team-based model. This year, I’ve seen in practice how collaboration among a multidisciplinary team improves patient care.
Host Site
5215 Centre Ave.
Pittsburgh, PA 15232
5215 Centre Ave.
Pittsburgh, PA 15232
